Beyond the Rash: Soothing Post-Herpetic Neuralgia After Shingles
Posted by Dennis R. Escalera on 28th Apr 2025
What Is Post-Herpetic Neuralgia?
Post-herpetic neuralgia (PHN) is a lingering, often debilitating nerve pain that can develop after an outbreak of shingles. Shingles, caused by the reactivation of the varicella-zoster virus (the same virus responsible for chickenpox), typically appears as a painful, blistering rash. While the rash fades in a few weeks, PHN occurs when nerve fibers remain damaged, causing ongoing burning, stabbing, or tingling sensations in the affected area.
PHN is one of the most common complications of shingles. While most people recover fully from shingles, around 10–18% of individuals, especially those over 60, may develop post-herpetic neuralgia that lasts for months—or even years—after the rash resolves.
Causes and Risk Factors
When the varicella-zoster virus becomes active again, it travels along nerve pathways and causes inflammation. During the healing process, some nerves don’t recover properly, leading to faulty signals between the skin and brain. This causes the brain to interpret normal sensations as pain—a phenomenon known as neuropathic pain.
Major Risk Factors:
- Age over 50
- Severe or prolonged shingles rash
- Delay in treating shingles
- A weakened immune system
- Pre-existing chronic pain conditions
Recognizing the Symptoms of PHN
The discomfort of PHN is very different from regular muscle or joint pain. It’s often described as:
- Burning or stabbing pain
- Sensitivity to touch (even clothing or a breeze can trigger pain)
- Persistent itching or tingling
- Numbness in the affected area
- Shooting electric-like sensations
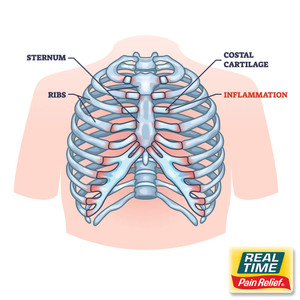
Pain typically stays localized to the area where the shingles rash occurred, most often on the torso, neck, or face.
How is PHN Treated?
There is no one-size-fits-all treatment for post-herpetic neuralgia. Since it involves nerve damage, treatment focuses on managing pain, reducing inflammation, and supporting nerve healing.
1. Medications
- Anticonvulsants such as gabapentin or pregabalin can calm overactive nerves.
- Antidepressants, including amitriptyline and nortriptyline, may change how the brain perceives pain.
- Topical patches, such as lidocaine, numb the area temporarily.
- Capsaicin cream, derived from chili peppers, may desensitize nerves when used consistently.
2. Nerve blocks or injections
In more severe cases, corticosteroid injections or nerve block procedures may be offered for short-term relief.
3. Topical Pain Relief Creams with Nature’s Ingredients
Many individuals prefer topical formulations made with botanical ingredients as a gentler, skin-soothing alternative—especially for long-term use. These creams can reduce inflammation, numb nerve endings, and support localized healing without harsh side effects.
Support from Nature’s Ingredients in Topical Formulations
The skin affected by PHN is often sensitive and inflamed, making gentle, plant-based ingredients ideal for relief. Applied topically, these components penetrate the skin to calm irritated nerves, reduce pain, and improve comfort.
? Arnica montana
Renowned for its use in treating bruises and nerve-related injuries, arnica offers anti-inflammatory and mild analgesic effects that may ease nerve pain when used as part of a gentle cream.
? St. John’s Wort
This herb has been traditionally used for nerve pain, especially in cases involving damaged or hyperactive nerves. It helps relax the nervous system and may ease hypersensitivity.
❄️ Menthol
Naturally cooling, menthol can provide temporary numbing and desensitize hypersensitive skin. It also helps “distract” the nervous system from pain by stimulating cold receptors.
? Calendula officinalis
This flower has skin-soothing and anti-inflammatory properties. When PHN causes dryness, itchiness, or irritation, calendula offers a layer of calming support.
? Witch Hazel
It acts as an astringent and anti-inflammatory agent that may reduce irritation and inflammation at the skin’s surface.
? Turmeric (Curcuma longa)
Its active compound, curcumin, has been shown to reduce inflammation and oxidative stress in nerve tissues. Topical application provides focused support without affecting the digestive system.
? Why Topicals Help
- Localized application targets the painful area directly
- Non-systemic—safer for long-term use
- Fast-acting and non-greasy
- Ideal for sensitive skin due to the gentle composition
Using these products regularly—2–3 times daily—can reduce surface pain, enhance circulation to damaged nerves, and support natural healing.
Lifestyle Tips to Help Manage PHN
Managing PHN often requires a multifaceted approach. In addition to creams and medications, these daily habits can support nerve health:
- Apply cool compresses to reduce burning sensations
- Wear soft, loose-fitting clothing to avoid friction
- Avoid stress which can amplify pain perception
- Stay hydrated and eat antioxidant-rich foods
- Engage in gentle movement or stretching to promote circulation
Prevention: The Shingles Vaccine
The Shingrix vaccine has been shown to significantly reduce the risk of both shingles and postherpetic neuralgia. It’s recommended for adults over 50 and those with weakened immune systems.
Vaccination is currently the most effective method of preventing the pain and complications associated with shingles.
Final Thoughts
Post-herpetic neuralgia can dramatically affect quality of life, especially when not managed early. Fortunately, topical relief options made with carefully selected plant-based ingredients offer a promising approach to ease daily discomfort, particularly for those with sensitive skin or other medical concerns.
By incorporating these options into a comprehensive care plan, individuals can regain control over their comfort and gradually return to the activities they love.